Vasectomy Reversal Claims that are Red Flags!
This article, written by Sheldon H.F. Marks, MD, discusses some of the issues and warning signs in 2023 that should be of concern by potential patients when discussing vasectomy reversals with doctors.
It is not wise to assume that all “vas reversal doctors” have the same training, do the same surgery, have the same skill, provide the same care before, during or after or know the same information. It’s always smart to ask questions and do research before making any decisions about which vasectomy reversal doctor is best for a couple.
Vasectomy reversals, like all highly technical surgeries, are not a cookbook, “one-size-fits-all” procedure. In fact, vas reversals are considered one of the most technically challenging surgeries that requires a deep understanding of male fertility and hormones as well as occupational, health and lifestyle influences on fertility (1). Each person, and in fact, each side of the vas, has to be individually evaluated for evidence that the vas is open and then to perform the correct reverse vasectomy technique specific to the findings on that side for that particular patient.
We teach at international courses that every patient should not automatically receive the exact same procedure, no matter what. The fact is that there is no way to know what technique, a vas-to-vas (VV) or vas-to-epididymal bypass (VE), will be needed beforehand (2) based on the number of years from vasectomy or from the exam. Plus, Dr. Marks just created the YouTube instructional video for other vas reversal doctors for the Society for the Study of Male Reproduction (SSMR).
 What is the correct way to assess the findings during the surgery and perform the appropriate vasectomy reversal technique needed?
What is the correct way to assess the findings during the surgery and perform the appropriate vasectomy reversal technique needed?
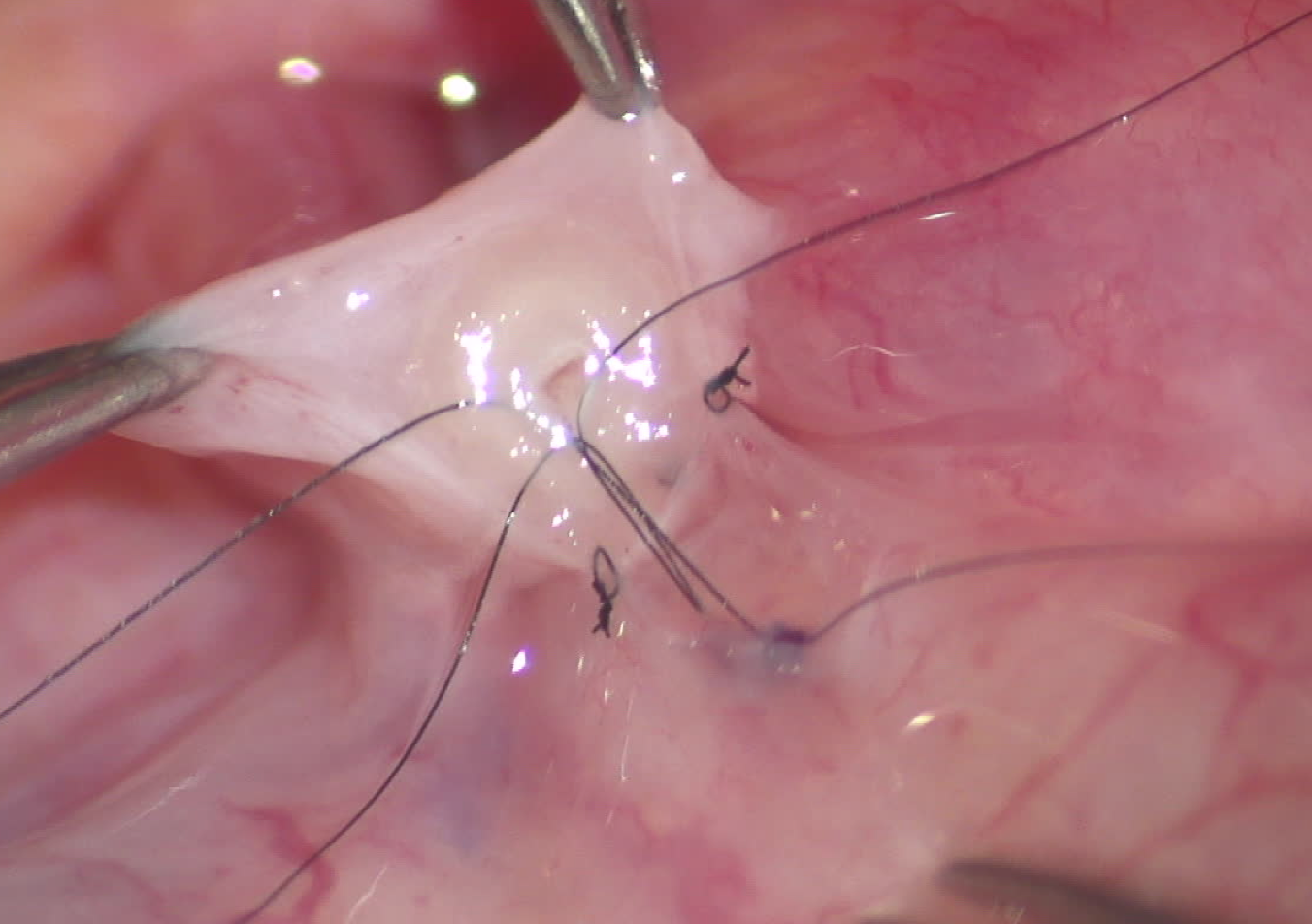
During each vasectomy reversal, a drop of the fluid that comes out of the vas is analyzed by our senior andrologist under a 400 power laboratory microscope. If whole sperm or sperm with long tails are seen, then we know that the tubes are open and the most up-to-date 3 to 4 multi-layer vas-to-vas connection is the correct repair. If we see creamy or paste-like fluid with no sperm and only debris or minimal, old degenerated heads, then this suggests that there is deeper blockage in the epididymis and then a more challenging vas-to-epididymal bypass (VE) is the correct technique that needs to be performed. Performing a vas-to-vas connection when no sperm are seen dramatically reduces the chance for success on that side, and most often zero success (3).
 We reinforce this key point to urologists in the classes we teach at international urology and fertility conferences, courses and even the textbook that we wrote for other vas reversal doctors (4). While a surgical resident at the Mayo Clinic in Rochester, Minnesota 40 years ago, the rule was “don’t start something unless it can be finished correctly.” That common sense rule still applies every time when performing a vasectomy reversal.
We reinforce this key point to urologists in the classes we teach at international urology and fertility conferences, courses and even the textbook that we wrote for other vas reversal doctors (4). While a surgical resident at the Mayo Clinic in Rochester, Minnesota 40 years ago, the rule was “don’t start something unless it can be finished correctly.” That common sense rule still applies every time when performing a vasectomy reversal.
But what if the doctor says what procedure that I will need before the vasectomy reversal?
This idea of knowing before is not accurate. We have analyzed the need for the straightforward vas-to-vas reversal vs. the epididymal bypass in thousands of men from 1 to 42 years out from their vasectomy. Yes, the chances for needing a bypass are usually very low in the first few years and go up at about 7 to 15 years from vasectomy and increase slowly, leveling off at about 20 to 22 years from vasectomy. What is also true is that there still a real chance that any individual patient may need an epididymal bypass on one or both sides starting anywhere from 2 years out from vasectomy.
There is absolutely no way to know beforehand based on the number of years from vasectomy which technique will be needed (5)! In fact, we just had a patient that had epididymal blockage only 2 years from vasectomy.
It is surprising that many patients receive the vas-to vas technique without the doctor even evaluating the vasal fluid microscopically, making the decision about what to do only on how the fluid looks or the numbers of years from vasectomy. I am confused when the fluid is analyzed by the doctor but then the patient still receives a vas-to-vas connection every time, no matter what is found in the vasal fluid, even if this is the wrong technique.
Just as worrisome are doctors that make claims of high vasectomy reversal success rates but don’t provide close after-care or monitor sperm counts afterwards. How does the doctor know his or her success if patients don’t obtain regular semen analysis tests? This should raise concerns.
Give us a call at (888) 722-2929 to find out the facts and why thousands of patients choose ICVR from every state in the US and more than 85 countries around the world.
We are also happy to set up a no cost, no obligation office, phone, Skype, Zoom or Face Time consult with one of our two microsurgeons to answer any questions.
This page was reviewed, edited and updated January 4, 2023 by Sheldon Marks, MD.
References:
1. Jurewicz J, Radwan M, Sobala W, Ligocka D, Radwan P, Bochenek M, Hanke W. Lifestyle and semen quality: role of modifiable risk factors. Syst Biol Reprod Med. 2014 Feb;60(1):43-51.
2.Kirby EW, Hockenberry M, Lipshultz LI. Vasectomy reversal: decision making and technical innovations. Transl Androl Urol. 2017 Aug; 6(4): 753–760).
3.Chawla A, O’Brien J, Lisi M, Zini A, Jarvi K. Should all urologist performing vasectomy reversal be able to perform vasoepididymostomies if required? J Urol 2004;172(3):1048- 50.
4.Marks SHF. Vasectomy Reversal: Manual of Vasovasostomy and Vasoepididymostomy. New York; Springer; 2018.
5.Mui P, Perkins A, Burrows PJ, Marks SF, Turek PJ. The need for epididymostomy at vasectomy reversal plateaus in older vasectomies: a study of 1229 cases. Androl 2014;2(1):25-9.