Vasectomy Reversals – A Step-by-Step Guide in 2023
The intent of this page, written by international authority, author and microsurgeon Sheldon H. F. Marks, MD, is to walk the reader through the vasectomy reversal experience, to better understand what is done and what to expect.
Getting started
Once each patient is comfortably sedated and asleep and the tissues are anesthetized with plenty of long acting local anesthetic, we draw out the segment of damaged vas (like a loop of spaghetti out of a button hole) through a very small “mini” incision in the front of the scrotum (1). Some doctors deliver the entire testicle and vas, but if not needed this seems more aggressive than necessary
 Prepping the vas
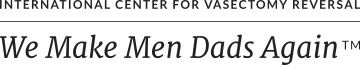
Prepping the vas
Using the Marks Vas Cutting Forceps, developed and tested here at ICVR, the vas is transected in the healthy tissue just above and below the vasectomy scar, which is then removed. If a sperm granuloma is present it is always removed.
Analyzing the fluid from the vas
A tiny drop of the fluid that comes out of the vas is then analyzed under a lab microscope (we have our own full-time andrologist to do this). If we see sperm or sperm parts, this confirms that the system is open and there is no deeper blockage, so a precision vas-to-vas connection is performed (2).
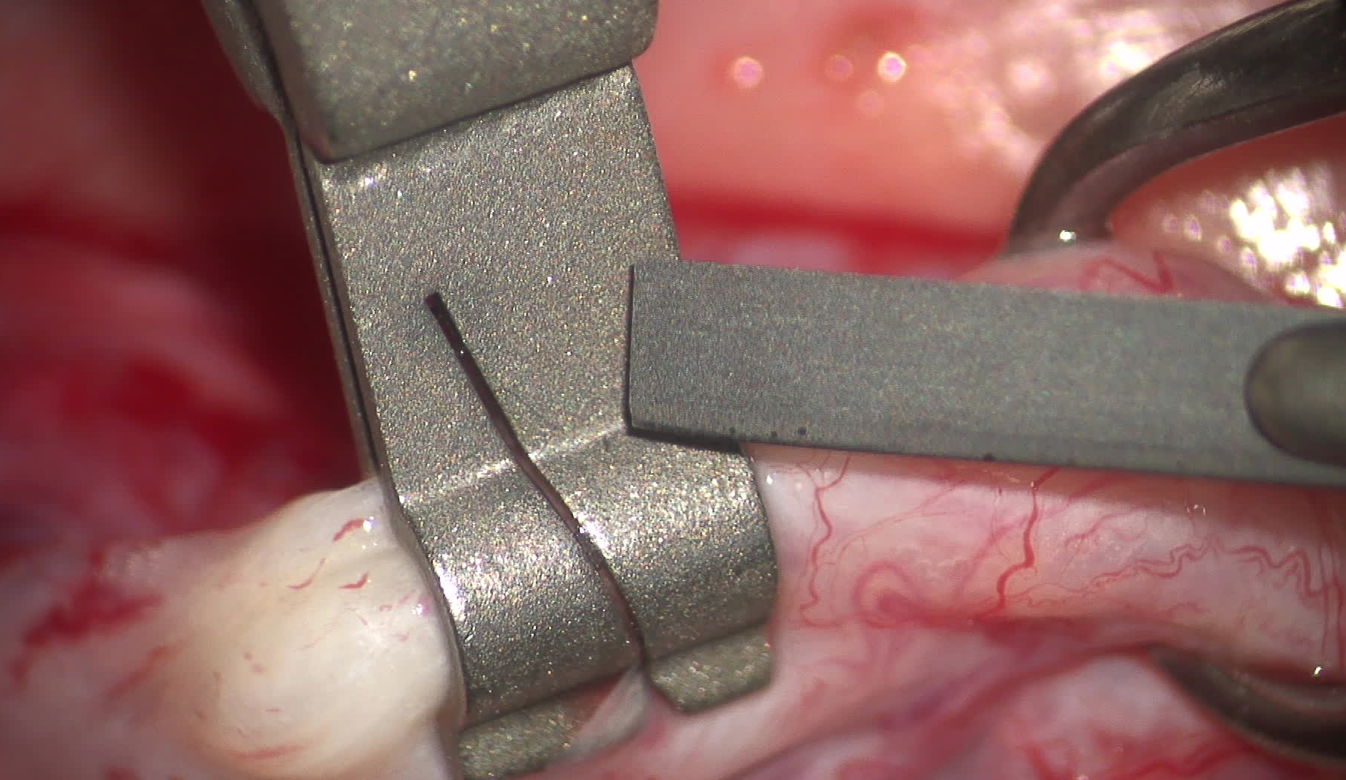
 The vas-to-vas connection
The vas-to-vas connection
A 3 to 4 multi-layer reversal is performed using our high-power Leica surgical microscope (3). The innermost layer on both sides is then sewn together with six or seven 10-0 nylon microsutures (each suture is a quarter thickness of an eyelash and about as long). The next muscular layer is connected with 15 or more individual 9-0 nylon sutures, each one millimeter apart, around the vas. Then the next layer or two of the outer tissues are than connected with multiple 7-0 nylon sutures to bring the blood supply over the connection and to secure and heal the repair site on no tension (4). This takes about 1 to 1.5 hours to do each side.
The other side, all over again
Once more numbing medicine is instilled into the tissues around the vas, the newly connected vas is placed back into the left side and this process repeated the very same way on the right side.
What if there’s no sperm in the fluid from the vas?
If we see no sperm in the vasal fluid, this usually tells us that there’s deeper obstruction in the epididymis from a blowout because of a buildup of pressure in the delicate thin-walled tubules and so a vas-to-epididymal bypass is needed (5). Many doctors can’t or won’t do this even though it is the only way the connection will work – they just do a vas-to-vas connection knowing there is probably very low chance for success (6).
The epididymis, where the blockage is located, is then examined under the high power surgical microscope. A single microscopic epididymal tubule above the blockage is opened to confirm sperm are present. Then the tiniest micro 10-0 nylon sutures are placed alongside the open tubule, which is drawn up into the end of the abdominal vas and secured in multiple layers. This also takes about 1 to 1.5 hours to perform on one side.
When finished, all the layers are closed individually and the skin closed, with the patient then walked to the adjacent recovery, feeling great and pain free!
During the vas reversal we call out to the family room regularly throughout the surgery with information to keep the wives up-to-date.
To answer any additional questions, set up a no-cost phone, Zoom, Skype, Face Time or office consult or to schedule a vas reversal, contact us at (888) 722-2929 .
This page was reviewed, edited and updated January 4, 2023 by Sheldon Marks, MD.
References:
1. Grober ED, Jarvi K, Lo KC, Shin E. Mini-incision vasectomy reversal using no-scalpel vasectomy principles: efficacy and postoperative pain compared with traditional approaches to vasectomy reversal. J.Urology. 2011;77:602–6.
2. Ramasamy R, Mata DA, Jain L, Perkins AR, Marks SH, Lipshultz LI. Microscopic visualization of intravasal spermatozoa is positively associated with patency after bilateral microsurgical vasovasostomy. Andrology. 2015 May;3(3):532-5.
3. Marks SHF. Vasectomy Reversal: Manual of Vasovasostomy and Vasoepididymostomy. New York; Springer; 2018.
4. Herrel L, Hsiao W. Microsurgical vasovasostomy. Asian J Androl. 2013 Jan;15(1):44-8.
5. Chan PT. The evolution and refinement of vasoepididymostomy techniques. Asian J Androl. 2013;15:49–55.
6. Chawla A, O’Brien J, Lisi M, Zini A, Jarvi K.Should all urologist performing vasectomy reversal be able to perform vasoepididymostomies if required? J Urol 2004;172(3):1048- 50.